The Language Of Pain - Tell A New Story
Let me explain that pain’s in your brain. How understanding pain science and how we talk about pain changes our perception and what we feel. This is some cool s**t
A great friend of mine who’s close to a decade older than me is a retired physiotherapist. Suffice it to say her job involved a lot of twisting and leaning over bodies and would’ve required a certain amount of physical strength.
She was one of the stalwarts in an adult contemporary dance class that I taught for yonks, was a Pilates client of mine, and frequented the gym. She’s always been very active; more than most people she knows the value of staying strong and fit especially as we age.
I think we’ve been conditioned to believe that knowledge is power and that the more information we can gather on a particular topic, the better.
Well…
My friend also happens to have scoliosis with all the physical ramifications it brings. I remember her once complaining about her hip to which I casually suggested that she should get a scan to “see what’s going on in there” to which she replied, “absolutely not!”
She knew that if she actually saw what was going on in there she’d embody it and then most likely be in greater pain and discomfort. Heck someone might even want to operate on her and in this, she was def not interested.
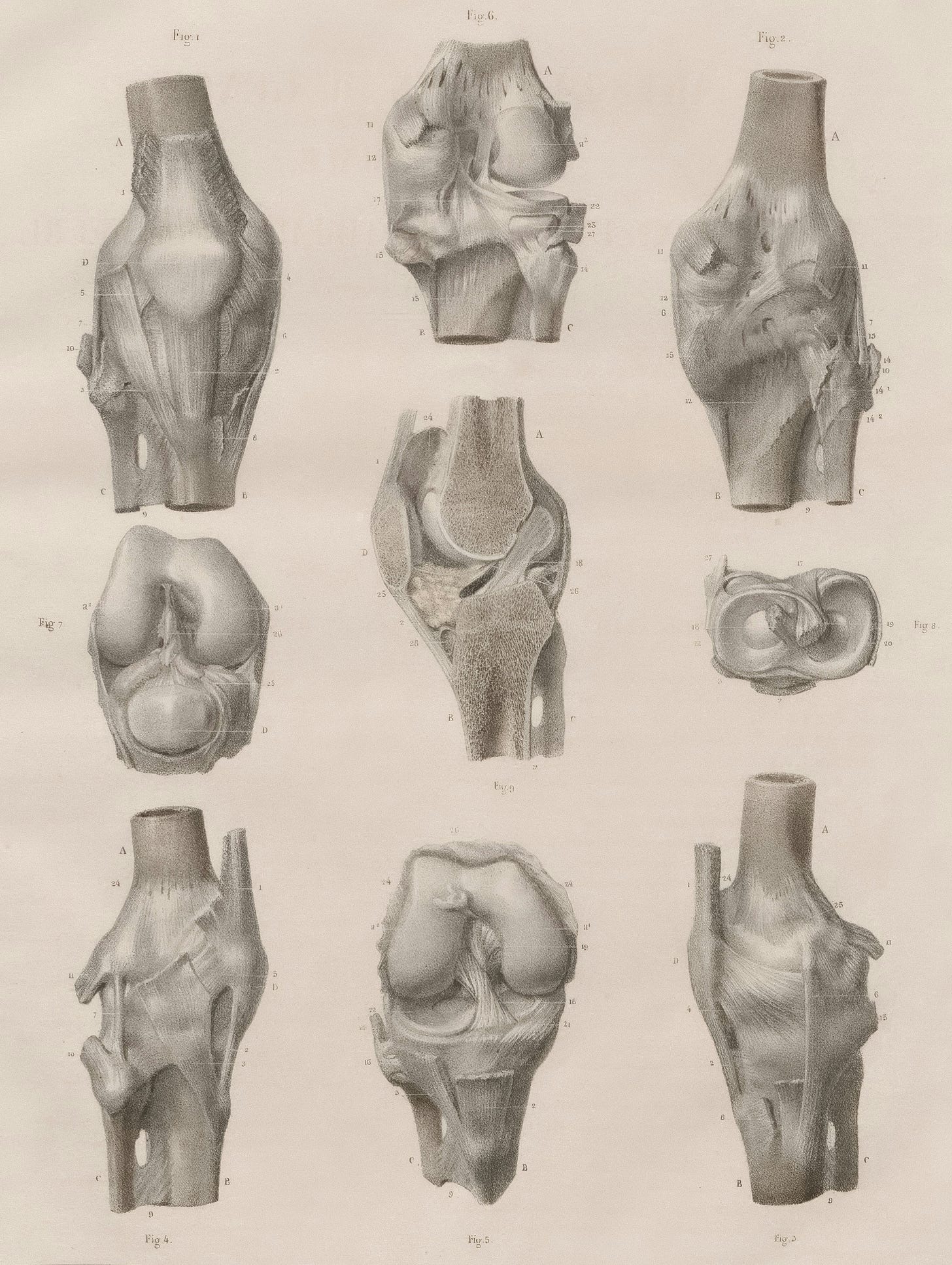
As many of you know last year I tore the medial meniscus of my right knee (or maybe it happened the year before? I ignored it for awhile a very long time). Once I got it looked at I was subsequently diagnosed with “severe” osteoarthritis. Now don’t those words conjure up some serious damage? And how about that old staple, “bone on bone”?
This was not exactly the news I hoped to hear and it immediately made me feel disappointed in the perceived failure and inevitable decline of my body.
My MD kindly asked if I wanted any other body part x-rayed to “see what was going in there because surely other joints were also arthritic, and wouldn’t I want to know that?”
I fervently declined.
Harkening back to my friend I knew I didn’t want to see what was going on in my body, especially in joints where I had no pain.
Not only didn’t I want to see, turns out I didn’t need to see.
I remember from past readings that research shows some people with intense low back pain have nothing out of the ordinary show up on their scans. Then there are other people who have zero, absolutely zippo pain. Their crappy ass scans show such degeneration that they shouldn’t be upright let alone obliviously moving through their world.
There’s an interesting research overview1 titled, Do not routinely offer imaging for uncomplicated low back pain. It examines the evolution of 20 years of research into the efficacy of using scans to treat people with low back pain. One of the things they found was that on scans (I’m assuming this means, x-rays, CTs and MRIs) 97% of people who were asymptomatic showed disc abnormalities.
So, to reiterate, these people had no symptoms yet their scans showed degeneration!
In these cases knowledge wasn’t power, instead ignorance was bliss.
It bears asking that if I’d seen evidence of arthritis and degeneration in my healthy, non-injured joints would I have started to feel pain in them?
Where Does Pain originate?
Pain is a signal in the brain!
Pain is a protective mechanism but sometimes that pain system can get overly sensitive, especially around an old injury.
We know that pain is elusive - it might hurt here (points to side of knee), or here (points to bottom of knee cap), or even here (points to back of knee). Pain tends to move around.
Sometimes a seemingly innocuous movement can set off a big wave of pain (or maybe it’s an I’ve been stabbed with a sharp kitchen knife type of pain - our body, it always keeps us guessing). The pain seems waaaaay out of proportion for what we’ve done.
Why is this?
Let me repeat myself.
Pain, which comes from the brain, is a protective mechanism that sometimes gets overly sensitive.
Some of that pain is anticipatory, we tell ourselves that “oh that movement hurts” or “it hurts when I do blah blah blah” and then when the pain happens it reconfirms our bias that moving in that way annoys our injured body part.
I know I’ve previously wondered if I was making something worse by doing x, y, or z. I felt that I wasn’t quite sure if I was causing more damage to the injured site and that made me tentative in my movements.
We also picture what our injured site looks like (“degeneration”, “severe”, “bone on bone”) and that makes us feel a certain way.
All these things build up our pain story.
It’s extremely hard to change this way of thinking, but there’s some good news.
A recent study2 has shown that if we understand pain science and also understand that generally movement is a good thing, then we can rewrite the story around our pain.
I love this name: The EPIPHA-KNEE Trial was done on knee osteoarthritis (you knew this blog post was all about me and my knee, right?). The trial looked at targeting unhelpful pain beliefs as a way to get people to exercise more.
Here’s what you need to know:
If we understand what’s going on in our brain it gives us greater capacity to break through the hyper-protective mechanism of our pain. Yes, in this case knowledge is power!
Other stressors in our lives can amplify our pain and we feel it more deeply.
The words we tell ourselves or are told by medical practitioners matter because we will believe them and then act (or not) accordingly.
Exercise (under the care of someone who knows what they’re doing) is good for us.
Loading the joint with weight bearing exercises is a way to increase blood flow and strengthening the muscles around the joint will help support the joint.
That’s right, we need to move and do exercise! When we seize up and stop moving we’re not doing ourselves any favours.
There is a term called bioplasticity which implies potential for improvement in all of the body’s systems. The evidence suggests that being diagnosed with arthritis does not necessarily signal a steady downward decline in use and function.
We’ll probably still be in pain but will be able to manage it more appropriately. We can all change how we interpret what we feel.
Didn’t I tell you it was cool s**t?
The Take Home Messages:
What YOU SEE & What YOU’RE TOLD Flows on to What YOU THINK and that Influences What YOU FEEL!
We can Tell a New Story. We can Change How we Interpret What we Feel.
Movement is Medicine!
Thanks for reading.
xBec
P.S. Two things to note:
I’m hosting a mini-retreat at my property in September, if you’re in the Gympie, Sunny Coast, or Brissie areas come on by: Move & Awaken Your Intuition will feature movement, a card reading workshop, and morning tea. Save 10% by July 16th with code, AWAKEN
Last week’s podcast episode was a cracker:
Hall AM, Aubrey-Bassler K, Thorne B, Maher CG. Do not routinely offer imaging for uncomplicated low back pain. BMJ. 2021 Feb 12;372:n291. doi: 10.1136/bmj.n291. PMID: 33579691; PMCID: PMC8023332.
Stanton TR, Braithwaite FA, Butler D, Moseley GL, Hill C, Milte R, Ratcliffe J, Maher C, Tomkins-Lane C, Pulling BW, MacIntyre E, Esterman A, Stanford T, Lee H, Fraysse F, Metcalf B, Mouatt B, Bennell K. The EPIPHA-KNEE trial: Explaining Pain to target unhelpful pain beliefs to Increase PHysical Activity in KNEE osteoarthritis - a protocol for a multicentre, randomised controlled trial with clinical- and cost-effectiveness analysis. BMC Musculoskelet Disord. 2021 Aug 28;22(1):738. doi: 10.1186/s12891-021-04561-6. PMID: 34454458; PMCID: PMC8401372.